HAS

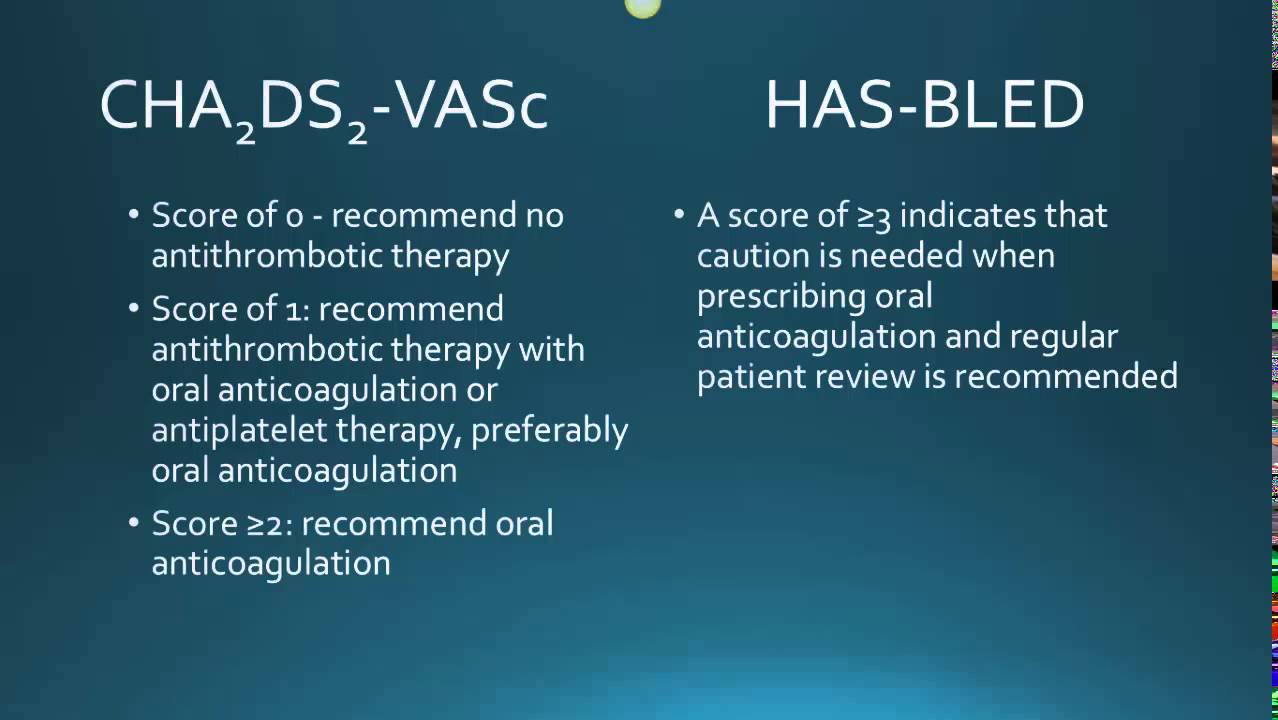
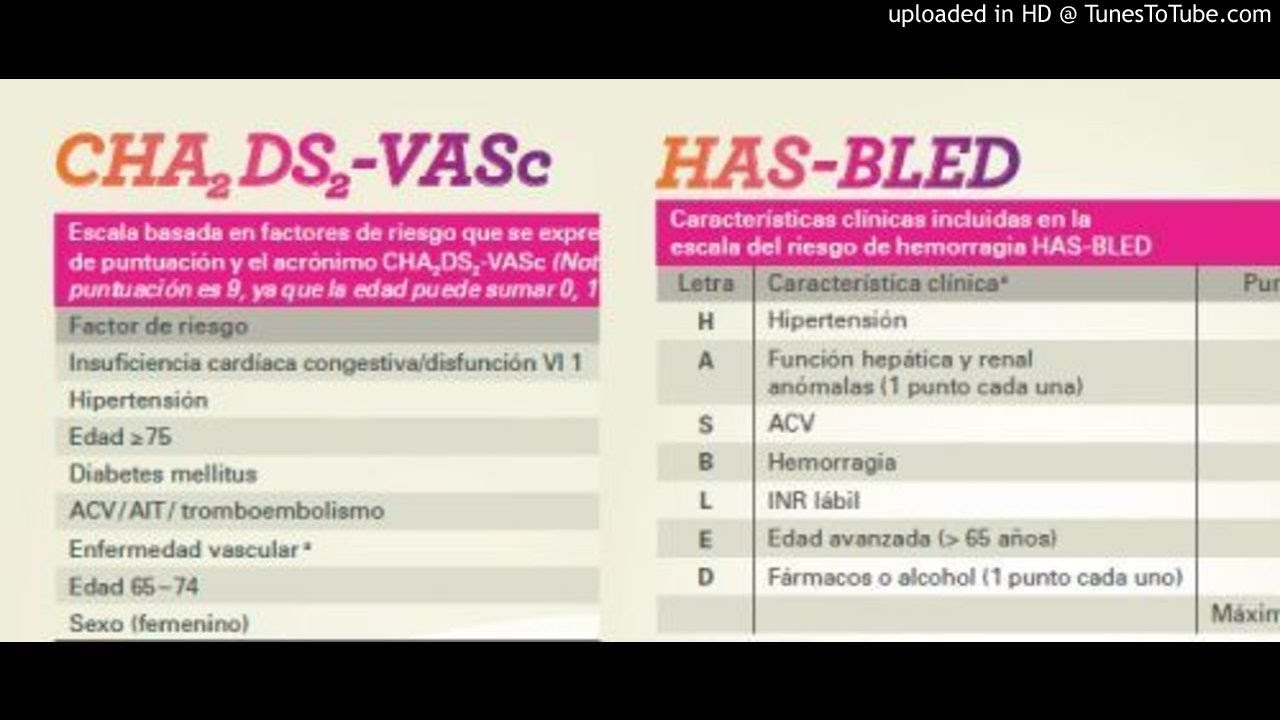
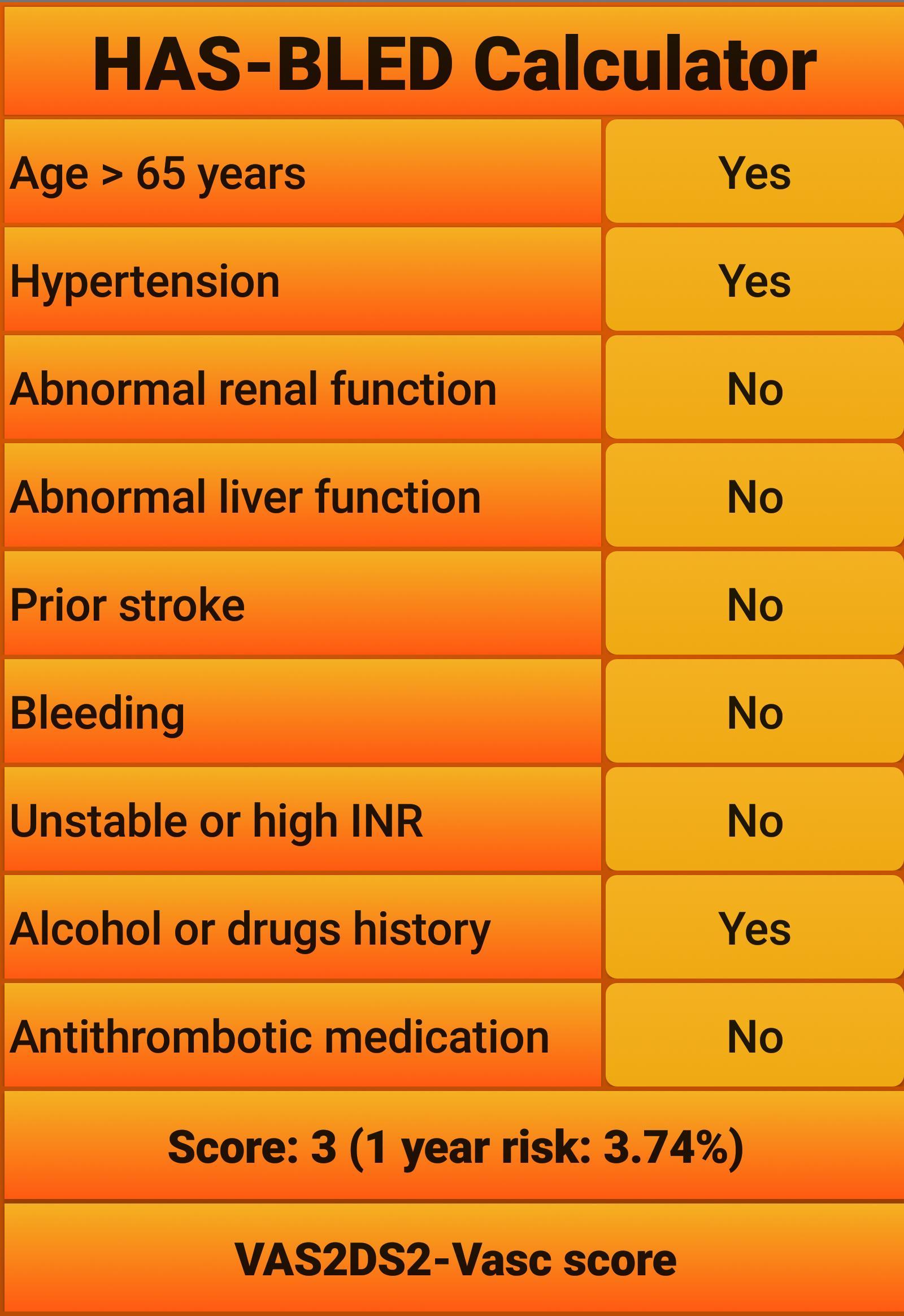
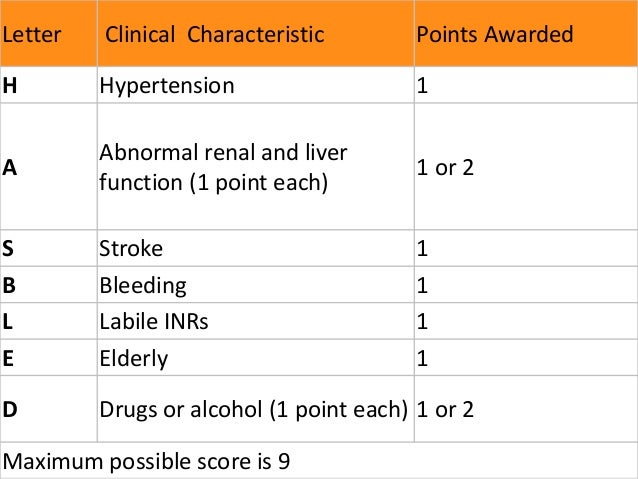
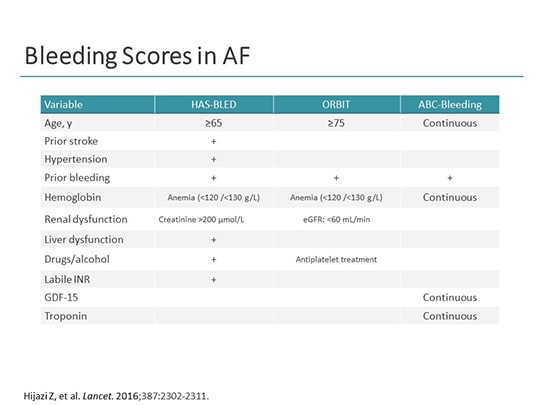
In clinical practice, we know that bleeding risk can be associated with a number of common clinical factors. A balance would be needed between simplicity and practicality—as well as predictive value, and as Zhu et al. Canadian cardiovascular society atrial fibrillation guidelines 2010: prevention of stroke and systemic thromboembolism in atrial fibrillation and flutter. . This score would help as a potential practical tool in clinical decision making, rather than 'guessing' the bleeding risk. It is recommended by the new European Society of Cardiology guidelines and the Canadian guidelines on atrial fibrillation management.
SPARCtool
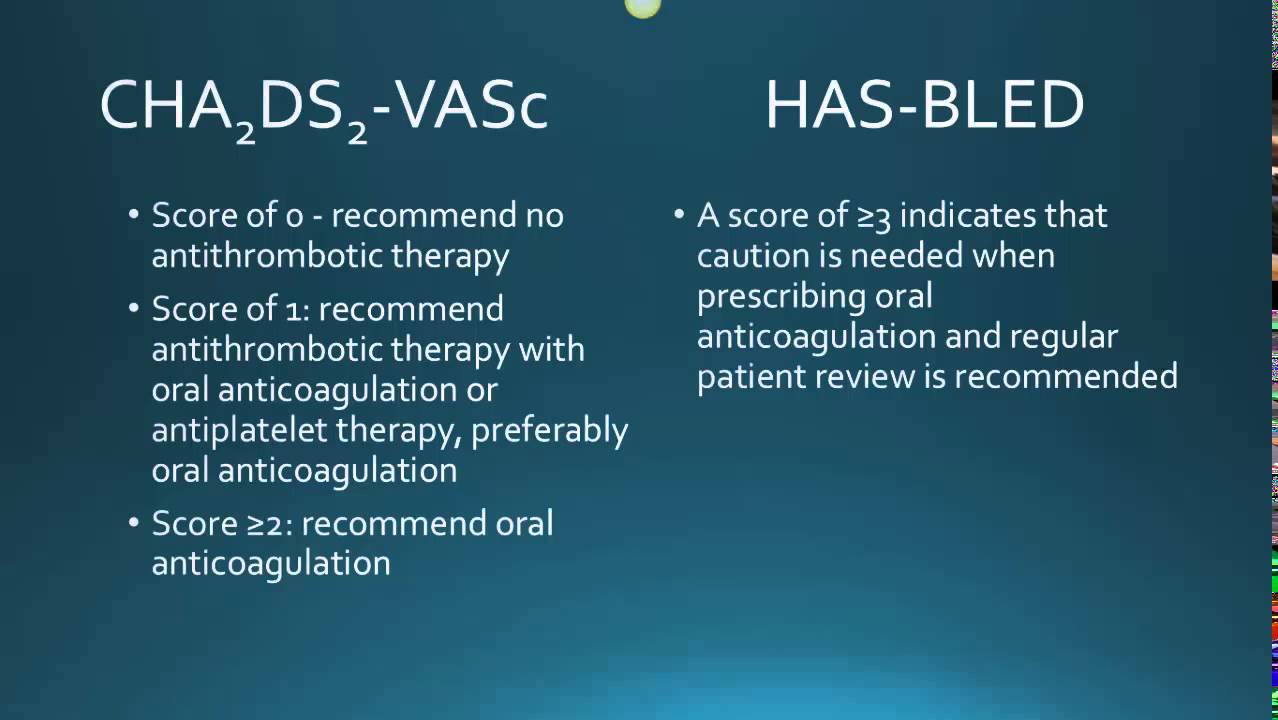
Bleeding risk assessment and management in atrial fibrillation patients. In a recent article validating the score, and were identified as additional risk factors for bleeding. However, would such an approach of adding additional tests help clinical application and practicality, or would oversimplification by reducing the number of clinical parameters really help the patient by misclassifying the patient as low risk? In the present issue of Clinical Cardiology, Zhu et al. The author has no other funding, financial relationships, or conflicts of interest to disclose. One can certainly add in biomarkers or imaging techniques eg, small vessel disease or microbleeds on cerebral imaging , but introduce additional complexity and costs of additional tests, with only a marginal improvement in predictive value, which may well be statistically significant; the clinical significance could be open to debate.
HAS

It is matched to the used for stroke risk stratification. Nonetheless, clinicians have been poor at estimating bleeding risk, with a tendency to overestimate risks in particular patients. . . .